Introduction to Amnesia
Amnesia, characterized by memory loss, can significantly impact daily life. From its symptoms to its various types and underlying causes, let’s delve into the comprehensive understanding of amnesia and explore preventive measures. Dissociative Amnesia, characterized by partial or complete loss of memory, poses significant challenges to individuals affected by it. Memory is a fundamental aspect of cognition, essential for various intellectual functions, making amnesia a condition of considerable concern.
Symptoms of Amnesia
The hallmark symptom of amnesia is memory loss, which can manifest in various ways:
- Difficulty recalling facts, events, or details.
- Impaired ability to learn new information.
- Confusion and disorientation.
- Inability to recognize faces or locations.
- Confabulation, where false memories are created to fill memory gaps.
While memory loss is prominent, individuals typically retain their motor skills and identity.
Verbal amnesia, where individuals struggle to recall words or names, is the most prevalent form of this condition. In rare cases, temporary memory loss may occur, leading to a complete blank in memory, including one’s identity and personal history. Poor memory resulting from brain weakness can manifest as mild headaches, noise intolerance, and difficulty concentrating.
Types of Amnesia
Amnesia encompasses several types, each with distinct characteristics:
- Retrograde Amnesia: Involves the loss of existing memories, with recent memories affected first. Conditions like dementia often cause gradual retrograde amnesia.
- Anterograde Amnesia: Prevents the formation of new memories, which can be temporary or permanent. Damage to the hippocampus, responsible for memory formation, can lead to permanent anterograde amnesia.
- Transient Global Amnesia (TGA): Characterized by temporary confusion and memory loss, often preceding a sudden onset. It is poorly understood and may result from brief disruptions in brain blood flow.
- Infantile or Childhood Amnesia: Commonly observed inability to recall early childhood memories, typically from the first 3 to 5 years of life.
- Dissociative Amnesia: Associated with traumatic events, causing memory gaps surrounding personal history or identity. It can be temporary or long-lasting.
- Post-Traumatic Amnesia (PTA): Following head injuries, individuals may experience memory loss surrounding the traumatic event’s timeframe. The duration of PTA correlates with the severity of the injury.
- Drug-Induced Amnesia: Temporary memory loss resulting from substances like benzodiazepines or general anesthesia medications.

Causes of Amnesia
Amnesia can stem from various underlying factors:
- Dementia: Progressive brain deterioration, often affecting recent memories first.
- Anoxia: Oxygen deprivation leading to temporary memory loss.
- Hippocampal Damage: Impairs memory formation and retrieval.
- Head Injuries: Trauma, stroke, tumors, or infections can cause permanent memory impairment.
- Alcohol Use: Short-term blackout or long-term Wernicke-Korsakoff syndrome.
- Trauma or Stress: Triggering dissociative amnesia or fugue states.
- Electroconvulsive Therapy (ECT): May induce temporary retrograde or anterograde amnesia.
The underlying causes of amnesia vary, ranging from biological factors to psychological influences. Brain cell impairment due to diseases or circulatory issues contributes significantly to memory loss. Additionally, psychological conditions like anxiety neurosis and traumatic experiences can impair memory function. Lifestyle factors, including dietary habits and overall brain health, also play a crucial role in memory maintenance.
Complications and Diagnosis
Even mild amnesia can disrupt daily activities and impact quality of life. Complications may arise from lost memories, potentially requiring continuous supervision. Diagnosis involves comprehensive evaluations by healthcare professionals, including cognitive tests and diagnostic imaging.
Treatment Approaches
Treatment focuses on addressing underlying causes and may include detoxification, medication, or occupational therapy. Preventive measures involve adopting a healthy lifestyle, including avoiding substance abuse, wearing protective gear, and staying mentally and physically active.
Nutrition plays a vital role in supporting mental health, and even minor nutritional deficiencies can exacerbate anxiety neurosis and memory issues. Individuals with amnesia should adhere to a balanced diet, avoiding stimulants like tea, coffee, and alcohol, while focusing on phosphorus-rich foods like cereals, nuts, and fruits.
Home remedies, such as the use of brahmi booti and almonds, offer natural solutions for memory enhancement. Herbal treatments and dietary supplements can also aid in strengthening brain function and improving memory retention. Furthermore, relaxation techniques like shavasana and meditation promote mental clarity and emotional balance, essential for memory enhancement.
Understanding Anterograde Amnesia: Symptoms, Causes, Treatment, Risk Factors, and Outlook
Anterograde amnesia is a condition characterized by the inability to form new memories, which can significantly impact daily functioning. From its symptoms to its underlying causes and potential treatment options, let’s explore this complex condition comprehensively.
Symptoms of Anterograde Amnesia
Anterograde amnesia primarily affects short-term memory processing, leading to difficulties in retaining new information. Common symptoms include:
- Forgetting recent encounters or conversations.
- Inability to recall recently learned information or phone numbers.
- Forgetting recent meals or changes in routines.
- Confusion and frustration due to memory lapses.
These symptoms differentiate anterograde amnesia from retrograde amnesia, which involves forgetting past events or established information.
Causes of Anterograde Amnesia
Brain damage, particularly affecting memory-making regions such as the thalamus, is the primary cause of anterograde amnesia. Factors contributing to brain damage include:
- Stroke
- Seizures
- Brain surgery or injury
- Brain tumors
- History of alcohol abuse
- Vitamin B1 deficiency
- Dementia
- Electroconvulsive therapy (ECT)
Diagnostic tests like MRI or CT scans help identify physical brain changes associated with anterograde amnesia.
Treatment Approaches
While there’s no cure for amnesia, treatments focus on improving quality of life and managing symptoms. Treatment options include:
- Vitamin B1 supplements to address deficiencies.
- Occupational therapy to enhance daily functioning.
- Memory training techniques.
- Technology assistance such as reminder apps.
Currently, there are no FDA-approved medications specifically for treating amnesia.
Risk Factors
Several factors increase the risk of developing anterograde amnesia, including:
- History of stroke, seizures, or brain injuries.
- Brain surgery or tumors.
- Alcohol abuse.
- Traumatic events like car accidents or sports injuries.
- Vitamin B1 deficiency.
- Undergoing electroconvulsive therapy (ECT).
The severity of symptoms depends on the extent of brain damage, with mild injuries potentially leading to temporary memory loss and more severe injuries causing permanent amnesia.
Outlook and Conclusion
Anterograde amnesia can be permanent, with symptoms potentially worsening over time. However, cases of temporary amnesia, such as transient global amnesia, may improve following an injury or illness. Seeking medical attention for unexplained memory loss or recent head injuries is crucial for accurate diagnosis and appropriate treatment recommendations.
Understanding the symptoms, causes, and treatment options for anterograde amnesia empowers individuals and their caregivers to manage the condition effectively and enhance overall quality of life.
Understanding Retrograde Amnesia: Types, Symptoms, Causes, Diagnosis, Treatment, and Outlook
What is Retrograde Amnesia?
Retrograde amnesia is a form of memory loss that impacts a person’s ability to recall memories formed before the onset of amnesia. It can result from various factors such as traumatic brain injury, illness, stroke, or degenerative brain diseases. Unlike anterograde amnesia, where new memories are affected, retrograde amnesia primarily disrupts access to pre-existing memories.
Types and Symptoms
- Temporally Graded Retrograde Amnesia: Typically, recent memories are affected first, while older memories remain intact. Symptoms include difficulty remembering events, names, faces, and facts from the past, while skills like driving or playing an instrument may be retained.
- Focal Retrograde Amnesia: This type involves isolated retrograde amnesia without significant anterograde amnesia symptoms. Memory loss is restricted to past events, leaving the ability to form new memories unaffected.
- Dissociative Amnesia: Resulting from emotional trauma rather than brain damage, this type causes memory gaps related to specific events, often temporary and linked to psychological shock.
Causes of Retrograde Amnesia
Various conditions can lead to retrograde amnesia, including traumatic brain injury, thiamine deficiency (often due to alcohol misuse or malnutrition), encephalitis, Alzheimer’s disease, stroke, seizures, and cardiac arrest. Each of these conditions affects different parts of the brain involved in memory storage and retrieval.
Diagnosis
Diagnosing retrograde amnesia involves a comprehensive medical examination, including imaging tests like CT or MRI scans, blood tests to check for deficiencies or infections, neurological evaluations, cognitive assessments, and EEG to detect seizure activity. It’s essential to provide accurate medical history details, possibly with the assistance of a caregiver.
Treatment
While there are no specific medications for treating retrograde amnesia directly, focusing on the underlying cause is crucial. For instance, managing conditions like epilepsy or providing support for degenerative diseases like Alzheimer’s can help mitigate symptoms. Occupational therapy, psychotherapy, and technology assistance, such as smartphones or tablets, can aid in memory rehabilitation and daily functioning.
Outlook
The outlook for retrograde amnesia varies depending on the underlying cause and severity. Some cases may improve over time, while others may remain stable or worsen. The support of loved ones and caregivers is essential in managing the challenges posed by retrograde amnesia, and with appropriate interventions, individuals can regain some level of independence and quality of life.
Understanding retrograde amnesia empowers individuals, caregivers, and healthcare professionals to navigate its complexities effectively, offering hope and assistance to those affected by this condition.
Conclusion
In conclusion, amnesia presents multifaceted challenges that require holistic management approaches. By addressing both biological and psychological factors through dietary modifications, herbal remedies, and relaxation techniques, individuals can improve memory function and enhance overall well-being.
Understanding Dissociative Amnesia: Types, Symptoms, Causes, Diagnosis, Treatment, Prognosis, and Key Takeaways
Dissociative amnesia is a complex mental health condition characterized by memory loss, often triggered by traumatic or highly stressful events. In this comprehensive guide, we delve into the various aspects of dissociative amnesia to provide valuable insights into its nature, causes, diagnosis, treatment, and prognosis.
Types of Dissociative Amnesia
Dissociative amnesia can manifest in several forms:
- Localized Amnesia: In this type, individuals cannot recall events from a specific time period.
- Generalized Amnesia: This rare form involves a complete loss of memory, including personal identity and life history.
- Fugue State: Individuals experiencing dissociative fugue may forget personal information and engage in unexpected travel or behavior.
Symptoms
Key symptoms of dissociative amnesia include:
- Memory loss, either complete or localized to specific events or periods.
- Association with trauma or stress, with memory gaps related to the triggering events.
- Duration of episodes, which can range from hours to weeks or longer.
- Inability to explain memory loss through other medical conditions.
Causes
Dissociative amnesia is closely linked to traumatic or intensely stressful experiences, such as abuse, combat, crime victimization, or natural disasters. The condition may result from the brain’s protective mechanism to dissociate from painful memories or the interference of stress with memory retrieval processes. Genetic predisposition may also play a role in some cases.
Risk Factors
Individuals who have experienced childhood abuse or significant trauma are at higher risk of developing dissociative amnesia. Additionally, certain comorbid conditions, including PTSD, depression, anxiety disorders, personality disorders, and substance use disorders, may coexist with dissociative amnesia.
Diagnosis
Diagnosing dissociative amnesia involves a comprehensive evaluation by healthcare professionals, including medical history assessment, physical examination, and psychological evaluation. Diagnostic tools such as the DSM-5 aid in identifying dissociative disorders and ruling out other causes of memory loss.
Treatment
Treatment aims to alleviate symptoms, facilitate memory recovery, and enhance coping mechanisms. Therapeutic approaches, including talk therapy, cognitive-behavioral therapy (CBT), and hypnosis, play a crucial role in addressing dissociative amnesia. While there are no specific medications for dissociative amnesia itself, medications may be prescribed to manage associated conditions like depression and anxiety.
Prognosis
The outlook for dissociative amnesia is generally favorable, with most individuals experiencing gradual or sudden memory recovery over time. Prompt treatment and addressing underlying traumas can significantly improve prognosis. However, the prognosis may vary based on the severity of amnesia, individual resilience, and adherence to treatment interventions.
Key Takeaways
- Dissociative amnesia involves memory loss without an underlying medical cause, often triggered by trauma or stress.
- Timely diagnosis and treatment are essential for managing dissociative amnesia and associated conditions.
- Recovery of lost memories can occur spontaneously or with therapeutic interventions.
- Seeking support from mental health professionals and loved ones can aid in coping with dissociative amnesia and promoting overall well-being.
By understanding the complexities of dissociative amnesia and addressing its underlying factors, individuals can embark on a journey towards healing and recovery.
Understanding Echoic Memory: How It Works, Examples, Duration, Factors, and Iconic vs. Echoic Memory
Echoic memory, a vital component of human memory, plays a crucial role in retaining auditory information for a brief period. In this informative guide, we explore the intricacies of echoic memory, its functioning, duration, real-life examples, factors influencing it, and its comparison with iconic memory.
How Echoic Memory Works
Echoic memory functions as a sensory register, capturing auditory information and temporarily storing it for further processing. When you hear a sound, the auditory nerve transmits the raw audio information to the brain. This information is then stored in the primary auditory cortex (PAC), where it remains for a few seconds before moving into short-term memory. The brain processes this information, giving meaning to the sound.
Examples of Echoic Memory
Echoic memory operates automatically, continuously storing audio information, even without conscious effort. Everyday scenarios where echoic memory comes into play include conversations, listening to music, and asking for repetition when distracted.
Duration of Echoic Memory
Echoic memory has a brief duration, typically lasting between 2 to 4 seconds. Despite its short lifespan, echoic memory enables the brain to retain auditory information temporarily, facilitating comprehension and recognition of sounds.
Factors Influencing Echoic Memory
Various factors can impact the efficacy of echoic memory. These include age, neurological disorders like Alzheimer’s disease or schizophrenia, substance use, hearing impairment, and language disorders. Additionally, characteristics of the sound itself, such as duration, frequency, intensity, volume, and language, influence echoic memory retention.
Iconic vs. Echoic Memory
While both iconic (visual) and echoic (auditory) memory are forms of sensory memory, they exhibit distinct characteristics. Iconic memory retains visual information for less than half a second, allowing for rapid processing of visual stimuli. In contrast, echoic memory lasts longer, accommodating the temporal nature of sound processing and enabling the retention of auditory information for a few seconds.
Seeking Help with Memory Issues
While occasional forgetfulness is normal, persistent memory problems warrant medical attention. Symptoms such as getting lost in familiar places, difficulty recalling common words, repeated questioning, slowed cognitive processes, and forgetting names of loved ones may indicate underlying issues. Consulting a healthcare professional, such as a psychologist or neurologist, can help diagnose and address memory-related concerns effectively.
Takeaway
Echoic memory serves as a crucial mechanism for retaining auditory information temporarily, contributing to our ability to perceive and comprehend sounds. While echoic memory is inherently short-lived, factors such as age and neurological conditions can influence its efficiency. Understanding the dynamics of echoic memory can aid in recognizing and addressing memory-related issues, ensuring optimal cognitive function and well-being. If you’re experiencing significant memory difficulties, seeking medical assistance is advisable for proper evaluation and management.
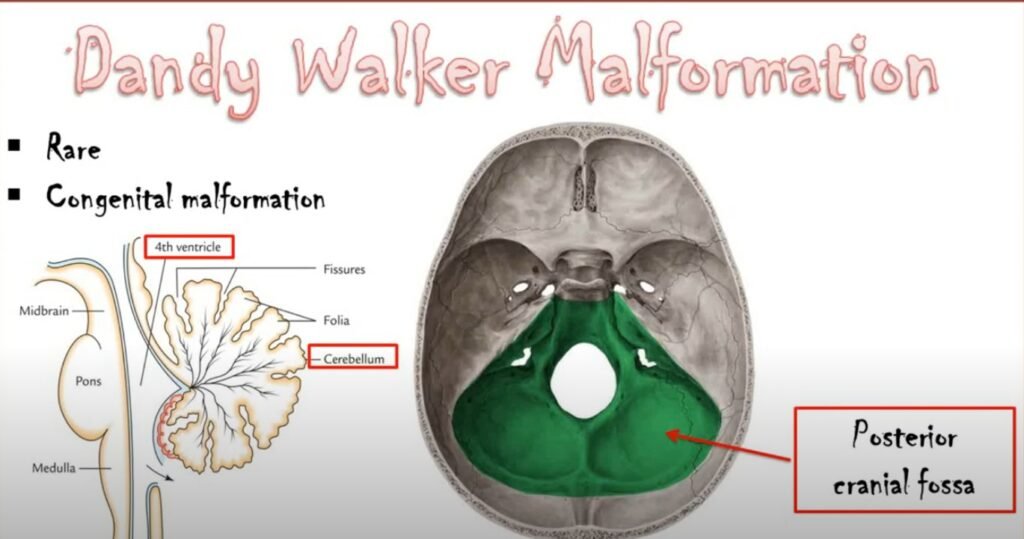
Understanding Dandy-Walker Syndrome: Symptoms, Causes, Diagnosis, Treatment, Outlook, and Takeaway
Dandy-Walker syndrome (DWS) is a rare congenital condition characterized by abnormalities in the development of the cerebellum, a part of the brain responsible for motor coordination and balance. In this comprehensive guide, we delve into the symptoms, causes, diagnosis, treatment options, outlook, and key takeaways related to Dandy-Walker syndrome.
Symptoms of Dandy-Walker Syndrome
DWS presents varying symptoms depending on the age of the individual. In infants, symptoms may include delayed motor skill development, difficulty controlling movements, and a larger than average head size. Older children may experience headaches, dizziness, vomiting, irregular eye movements, and challenges with balance and coordination.
Causes of Dandy-Walker Syndrome
The precise cause of DWS remains unclear, although genetic abnormalities are often associated with the condition. Factors such as maternal diabetes during pregnancy, a history of infertility, viral infections, and exposure to environmental toxins may increase the risk of DWS in infants. However, the overall likelihood of developing DWS remains low.
Diagnosis of Dandy-Walker Syndrome
DWS can sometimes be detected during pregnancy through ultrasound or fetal MRI scans, revealing abnormalities in the development of the cerebellum. Genetic testing may also identify underlying genetic factors contributing to the condition.
Treatment for Dandy-Walker Syndrome
Treatment for DWS focuses on managing the structural anomalies in the brain and alleviating associated symptoms. Surgical intervention may be necessary to remove excess fluid buildup and reduce pressure on the brain. Physical, occupational, and speech therapy can help address motor and cognitive challenges associated with DWS. Additionally, medications may be prescribed to manage conditions such as seizures or attention deficit hyperactivity disorder (ADHD).
Outlook for Individuals with Dandy-Walker Syndrome
The prognosis for individuals with DWS varies depending on factors such as the extent of cerebellar abnormalities, the presence of additional fluid buildup, and associated complications. While some individuals may experience mild symptoms and lead relatively normal lives, others may face significant physical and intellectual disabilities. Early detection and intervention play a crucial role in improving health outcomes and enhancing quality of life for individuals with DWS.
Key Takeaway
Dandy-Walker syndrome is a congenital condition characterized by abnormal cerebellar development, leading to challenges with motor coordination and balance. While there is no cure for DWS, early detection and multidisciplinary treatment approaches can help manage symptoms and improve overall well-being. Genetic counseling and prenatal screening may offer valuable insights for families at risk of DWS, facilitating informed decision-making and personalized care plans.

FAQs
- What are the common symptoms of amnesia?
- Common symptoms include difficulty recalling words or names, temporary memory loss, headaches, noise intolerance, and concentration issues.
- How can dietary changes help alleviate amnesia?
- Adhering to a balanced diet rich in phosphorus and avoiding stimulants like tea, coffee, and alcohol can support brain health and alleviate memory issues.
- Are there any natural remedies for improving memory?
- Yes, herbal remedies like brahmi booti and almonds, along with dietary supplements, can aid in memory enhancement and brain function improvement.
- How effective are relaxation techniques in managing ?
- Relaxation techniques such as shavasana and meditation promote mental clarity and emotional balance, essential for managing amnesia and improving memory function.
- What role does meditation play in memory enhancement?
- Meditation helps create balance in the nervous system, promoting hormonal balance and aiding in memory enhancement. Regular meditation practice can significantly improve memory retention and cognitive function.